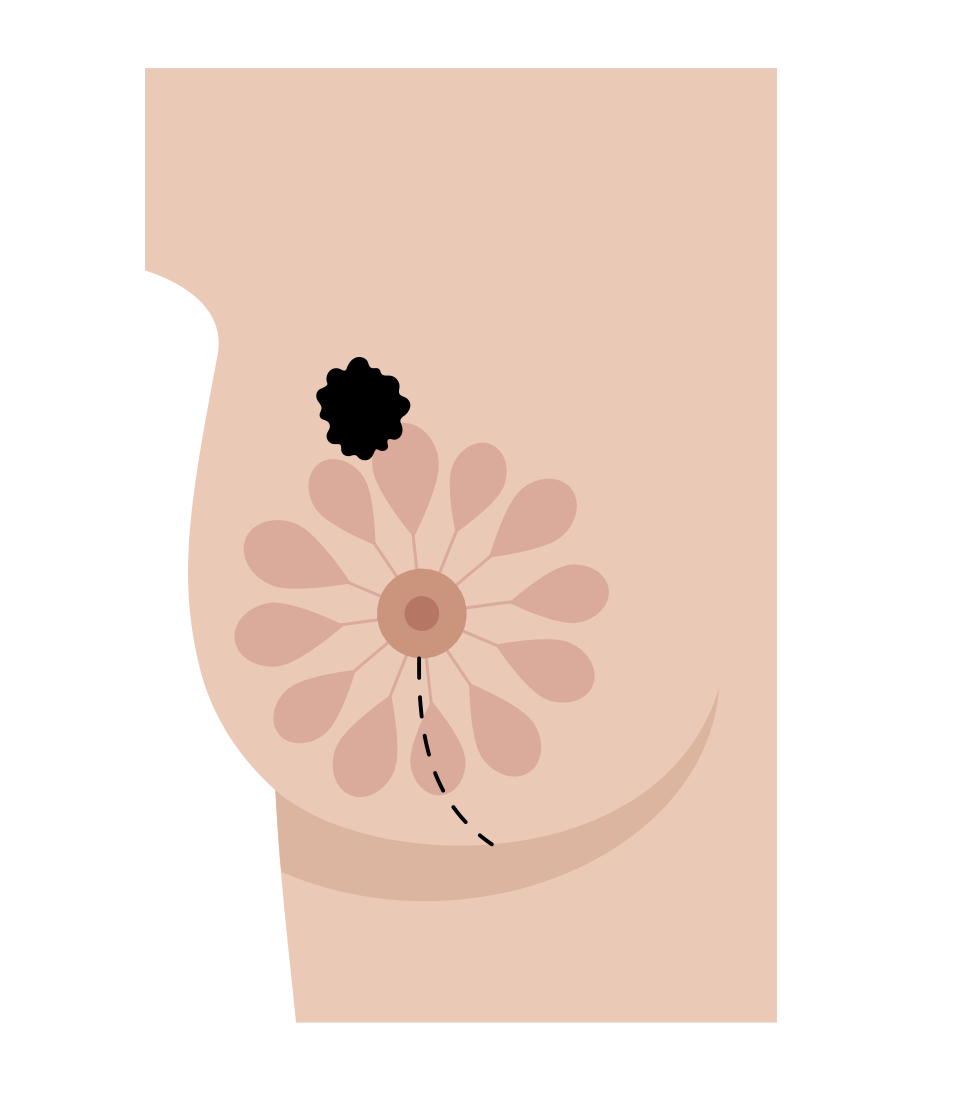
For a nipple-sparing mastectomy The surgeon removes:
All of the breast tissue, the nipple, areola, and the skin of the breast is left intact.
Lymph nodes are usually removed as well to see if the cancer has spread beyond the breast (unless the mastectomy is prophylactic).
Either a sentinel lymph node dissection or an axillary lymph node dissection will be done depending on your specific diagnosis. Also, some tissue from beneath the nipple and areola is removed to check for cancer cells there. If cancer is found in that location, the nipple and usually the areola will need to be removed. This is usually done later on, in a separate procedure. Another reason the nipple may need to be removed in a separate procedure is if it does not have a good enough blood supply and develops necrosis (tissue breakdown).
Also, some tissue from beneath the nipple and areola is removed to check for cancer cells there. If cancer is found in that location, the nipple and usually the areola will need to be removed. This is usually done later on, in a separate procedure. Another reason the nipple may need to be removed in a separate procedure is if it does not have a good enough blood supply and develops necrosis (tissue breakdown).
In most cases, the breasts are immediately reconstructed during a nipple-sparing mastectomy, with either tissue expanders, breast implants, or tissue flaps. If the nipples need to be removed, they can be reconstructed at a later point with nipple reconstruction surgery, nipple tattoos, or both.

The procedure is appropriate for women who have a strong family history of breast cancer or who carry the BRCA gene mutation and are seeking a risk reduction preventive (“prophylactic”) mastectomy
You might be a candidate for a nipple-sparing mastectomy if:
You are planning on having immediate breast reconstruction, meaning that you will have one surgery in which both the mastectomy and breast reconstruction are performed;
Your cancerous cells are relatively small;
Your cancerous cells are located several centimetres away from the nipple;
You have small or medium-sized breasts;
You do not have large or sagging breasts, as it can be difficult to reposition the nipple on breasts with these characteristics; and
You are having a mastectomy to remove existing cancer, and not having a mastectomy due to preventative reasons.
A mastectomy without immediate breast reconstruction can take 1-3 hours. If immediate breast reconstruction is performed during the mastectomy, the surgery will take longer (about 3 to 4 hours for reconstruction with tissue expanders or breast implants and 6 to 8 hours for reconstruction with tissue flaps).
During the mastectomy, the surgeon separates the breast tissue from the skin and muscle. All of the breast tissue that the surgeon can see — which lies between the collarbone and ribs, from the side of the body to the breastbone in the center — is removed. Depending on the type of mastectomy you are having, your surgeon may remove other parts of the breast.
You will have drains in each operated breast and stay overnight in the hospital. Most patients complain of chest tightness after this surgery. You will be prescribed muscle relaxants that will help with the tightness.
Taking pain medication
Caring for the bandage (dressing) over your incision, surgical drain and stitches.
Recognising signs of infection-fever, increased redness around the incision, and pus draining from the incision.
Exercising your arm ( In case SLNB or ALND was performed)
Recognising signs of lymphedema ( In case SLNB or ALND was performed)
You can wear a breast prosthesis or bra after the wound heals.